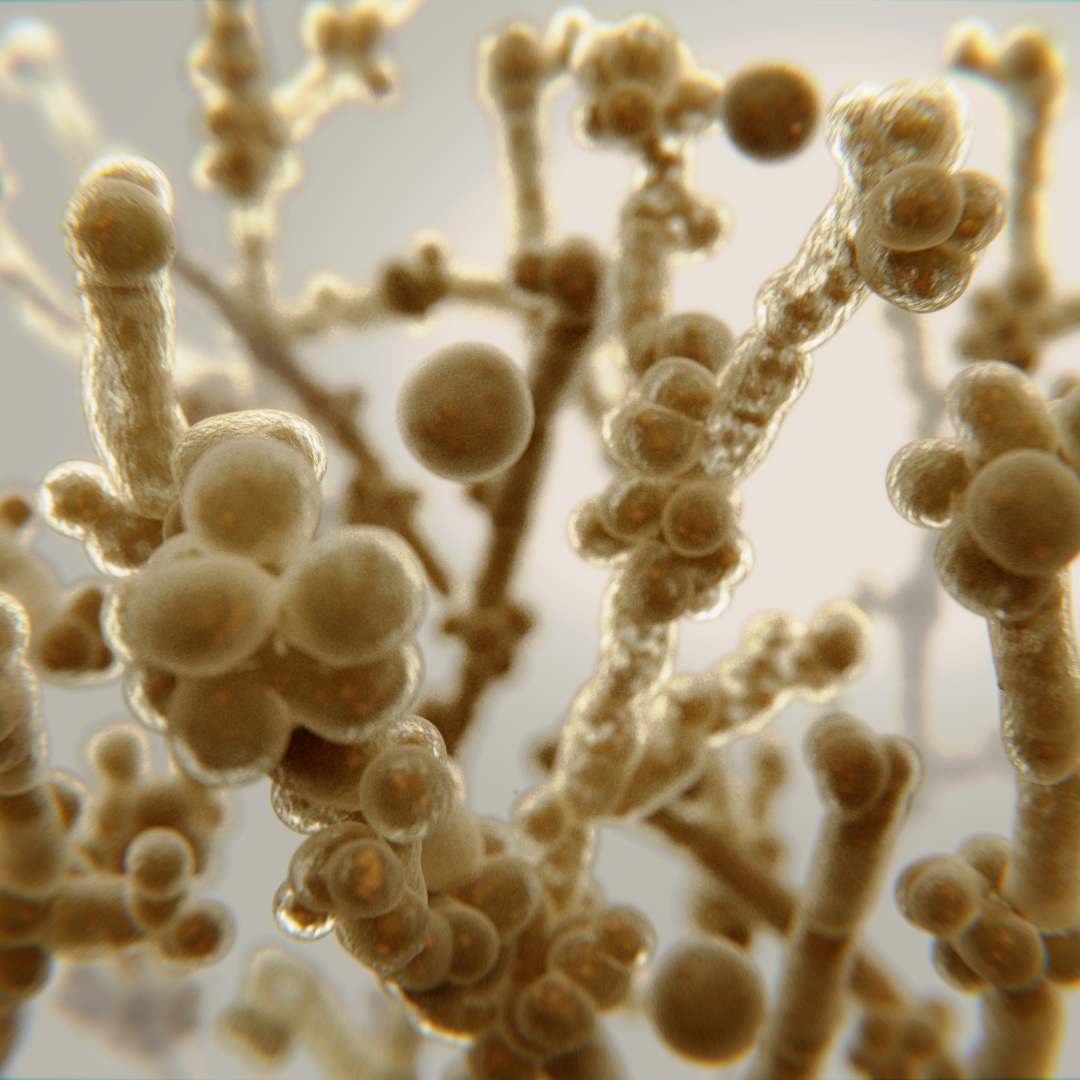
Fungal Pandemic – Could it Happen?
April 28, 2023
Lyme Disease
May 18, 2023TRENDING WELLNESS TOPIC: HOSPITAL CODING AND DOCUMENTATION
What is the problem?
Inpatient physicians find clinical documentation queries irritating and unnecessary! These time-consuming documentation queries can be avoided through education and improved protocols. Hospitals have identified a need for clinical documentation education from various perspectives, such as continuity of care, support of medical necessity/severity of illness/risk of mortality, medical-legal, and support of diagnosis and evidence of compliance with Core Measures. Observations have highlighted that various charting and documentation errors are prevalent across all disciplines and units. These issues exist in all hospitals and departments because the terminology and the rules put forth by CMS constantly change. Documentation must be comprehensive enough and sufficient enough to document the patient’s history and physical, progress notes, consultations, etc. Often the same information is repeated with little change throughout the stay. Understanding how what a physician document in the chart directly affects ICD-10 codes, quality data, research, and reimbursement is important.
Learning Objectives
1. Describe how to avoid the most common types of Clinical Documentation Queries through improved documentation
2. Explain how physician notes are turned into ICD-10 codes
3. Describe why Present on Admission conditions are essential to document
CLICK HERE to download a PDF file featuring information gaps, potential needs, and references for this topic.
If your medical staff needs an update on improving documentation, consider contacting our office to book a speaker at 877-505-4777 or info@speakersnetwork.com.

info@speakersnetwork.com
REFERENCES





